📌 Introduction – What You Need to Know
Obesity is one of the greatest health epidemics of our time. What many people don’t realize is that obesity can increase the risk of dementia and other brain-related problems. Recent research shows that belly fat and central obesity are particularly linked to changes in the brain, especially in gray matter, a critical area for memory, thinking, and learning.
In this article, we explain step by step what obesity does to your brain, why central belly fat is different from evenly distributed body fat, how gray matter and brain volume may be affected, and what scientific evidence shows. We also cover what you can do to reduce the risks, how diet and lifestyle help, and answer the most important FAQs.
🤔 What Is Obesity?
Obesity is a chronic condition characterized by an excess of body fat. It is usually measured with the Body Mass Index (BMI), but this measure doesn’t tell the full story. The location of fat accumulation, such as fat around the abdomen, is especially important for health outcomes.
🧬 Central vs. Evenly Distributed Fat
Fat that is evenly distributed across the body (such as under the skin) is less harmful than fat stored around the belly. This is called central obesity or abdominal obesity, which appears to be more dangerous for heart disease, diabetes, and possibly brain health.
🧠 How Obesity Can Affect the Brain
🔹 Gray Matter vs. White Matter
The brain consists of two major types of tissue:
-
Gray Matter: Composed of neuronal cell bodies, crucial for thinking, memory, and information processing.
-
White Matter: Made up of axons that allow communication between brain regions.
Recent research shows that central obesity is mainly associated with a decrease in gray matter volume, while white matter seems less affected.
A UK study involving nearly 10,000 participants found that people with a higher waist-to-hip ratio had lower gray matter volume compared to those without central obesity.
This indicates that not all forms of obesity have the same impact on the brain—the location of fat matters.
Note: Gray matter in the brains of Britons with excess belly fat was nearly 2% lower than in participants without central obesity.
Additionally, for obese individuals with more evenly distributed body fat, the “lost” gray matter volume was much smaller compared to the control group.
Obesity as a Risk Factor for Diseases
Obesity is a known risk factor for many diseases, including age-related conditions. However, it is still unclear whether it directly affects brain disorders. To investigate this, researchers at University College London examined whether brain volume depends on overweight status. They analyzed a sample of 9,652 people from the UK Biobank Study (2006–2010), which recruited volunteers to study complex age-related diseases.
Obesity was measured using BMI (weight in kg ÷ height in meters²), with a BMI over 30 classified as obesity. To determine obesity type, researchers calculated the waist-to-hip ratio (waist circumference ÷ hip circumference). Ratios above 0.9 for men and 0.85 for women indicated central obesity, where fat accumulates around the abdomen.
Brain volume was measured using MRI, separately assessing gray matter (neuronal cell bodies) and white matter (axon pathways). Participants also provided information on health, lifestyle, and habits.
After controlling for factors like smoking and high blood pressure, researchers found that gray matter volume reduction was localized to specific parts of the striatum—a deep brain structure involved in conditioned reflexes and internal organ regulation—while white matter remained intact.
-
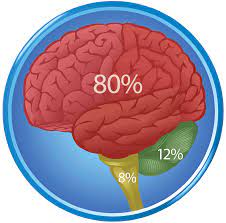
Non-obese participants: ~798 cm³ gray matter volume
-
Slightly overweight participants: ~793 cm³
-
Obese with evenly distributed fat: little difference from non-obese
-
Obese with central obesity: ~786 cm³, nearly 2% less gray matter
This shows that central obesity correlates with gray matter loss. It is premature, however, to claim a causal link. Does obesity reduce gray matter, or does reduced gray matter contribute to belly fat accumulation?
Since brain shrinkage is associated with dementia and memory loss, obese individuals may also be at risk. Researchers note that their data represents only 5% of the obese population and that participants were generally healthier than the average obese Briton.
🧪 What Does the Research Show?
📊 Key Findings from UK MRI Studies
-
Overall brain size did not significantly differ between groups.
-
Participants with central obesity had significantly less gray matter in certain brain regions.
-
Gray matter reduction was most notable in the striatum, which plays a role in memory, motivation, and behavior.
It’s important to emphasize that obesity is not proven to directly cause brain shrinkage; the link is correlational, and genetic and environmental factors may also play a role.
🧠 How Gray Matter Loss Increases Dementia Risk
Gray matter is critical for cognitive functions such as:
-
Memory
-
Learning
-
Language skills
-
Problem-solving
Gray matter loss is commonly seen in neurodegenerative diseases like Alzheimer’s and dementia. Greater loss increases the risk of cognitive decline.
Thus, central obesity and excess belly fat are concerning because they may alter brain anatomy and contribute to an increased dementia risk.
🧠 Other Research on Obesity and the Brain

Reactive Brains in Obesity
Beyond structural changes, research shows that the brains of people with obesity respond differently to food cues. A Dutch study found that people with obesity are slower to feel satiated, which can lead to:
-
Increased food intake
-
Difficulty losing weight
-
A vicious cycle of obesity
These differences are also measurable in brain activity and dopamine signaling in the reward system, influencing eating behavior. Other studies show that the brains of obese individuals respond less effectively to appetite-suppressing signals, making long-term behavior change difficult.
🧠 Other Factors Affecting Brain Health
Obesity doesn’t act alone—other factors also contribute to cognitive decline:
-
Lifestyle: Nutrition, sleep, stress, physical activity, and social interaction affect brain function.
-
Genetics: Genetic variants may increase susceptibility to obesity and neurodegenerative diseases.
-
Inflammation & Metabolism: Chronic inflammation from obesity can impair brain function.
🍎 What You Can Do
✔️ Healthy Diet
An anti-inflammatory diet rich in vegetables, fruits, fish, fiber, and healthy fats supports both weight management and brain health.
✔️ Exercise
Regular physical activity improves:
-
Blood flow to the brain
-
Memory and cognitive function
-
Glucose and fat metabolism
✔️ Sleep & Stress Management
Chronic sleep deprivation and stress worsen metabolic and hormonal imbalance, affecting cognitive function.
📚 External Resources & Further Reading
🔗 👉 Time – Body Fat May Affect Your Brain Volume, Study Says – Summary of research showing how higher body fat—especially around the waist—is linked to lower gray matter volume in the brain, clarifying that the study shows association, not causation.
🔗 👉 Alzheimer’s Society – Obesity and Dementia Risk – Explains how obesity during mid‑life increases dementia risk later in life, highlighting connections with metabolic conditions like diabetes, blood pressure, and inflammation.
🔗 👉 AARP – How Being Overweight Can Affect Your Brain Health – Discusses research showing that excess weight is associated with reduced brain volume and lower blood flow to the brain, factors linked to cognitive decline and dementia.
💊 Anti‑Obesity Medications
🔗 ScienceDirect: Obesity medications: A narrative review of current and emerging agents – An overview of medications approved for obesity management, highlighting how these drugs support long‑term weight loss when combined with lifestyle changes and discussing their effectiveness and safety.
❓ Frequently Asked Questions (FAQ)
📌 1. Does obesity really increase dementia risk?
Evidence suggests central obesity may lead to structural brain changes that raise dementia risk, but there is no definitive causal proof.
📌 2. Why is belly fat more dangerous than fat elsewhere?
Abdominal fat produces hormones and inflammatory factors affecting metabolism and possibly brain function.
📌 3. Can weight loss reduce gray matter loss?
Studies suggest weight loss and a healthy lifestyle improve metabolic and brain health, though long-term human evidence is limited.
📌 4. What role does gray matter play in cognitive function?
Gray matter contains neuronal cell bodies essential for memory, learning, planning, and emotional regulation.
📌 5. Can children also experience obesity-related brain changes?
Some research suggests childhood obesity may affect cognitive performance and brain function, though more studies are needed.
🧾 Conclusion
Obesity is not just a matter of weight. Central obesity and excess belly fat are associated with brain changes, especially gray matter loss, which may contribute to increased dementia and cognitive decline risk.
While researchers cannot yet claim that obesity directly causes brain shrinkage, multiple correlations indicate potential harmful effects. Therefore, preventive steps like a healthy diet, sufficient sleep, physical activity, and stress management are crucial.
🧠 Further Reading & Resources. Explore more on the AlexWaterandBouw Blog – Health Category for information on health, nutrition, and lifestyle impacts on the body. For example, read the article How to Reduce Daily Stress with Simple Habits to learn practical strategies that support both brain and body health.


